Understanding Polycystic Ovary Syndrome (PCOS) and How It Affects Fertility
“You’ve got PCOS.”
It’s a phrase many patients hear in fertility clinics—but often without a clear explanation of what it means, what to expect, or what comes next.
Polycystic Ovary Syndrome (PCOS) is the most common endocrine disorder among women of reproductive age, affecting approximately 1 in 10 individuals. Despite being so widespread, PCOS remains one of the most complex and misunderstood conditions in reproductive health.
At Indiana Fertility Institute (IFI), we’re here to break it down and support you every step of the way.
What is PCOS?
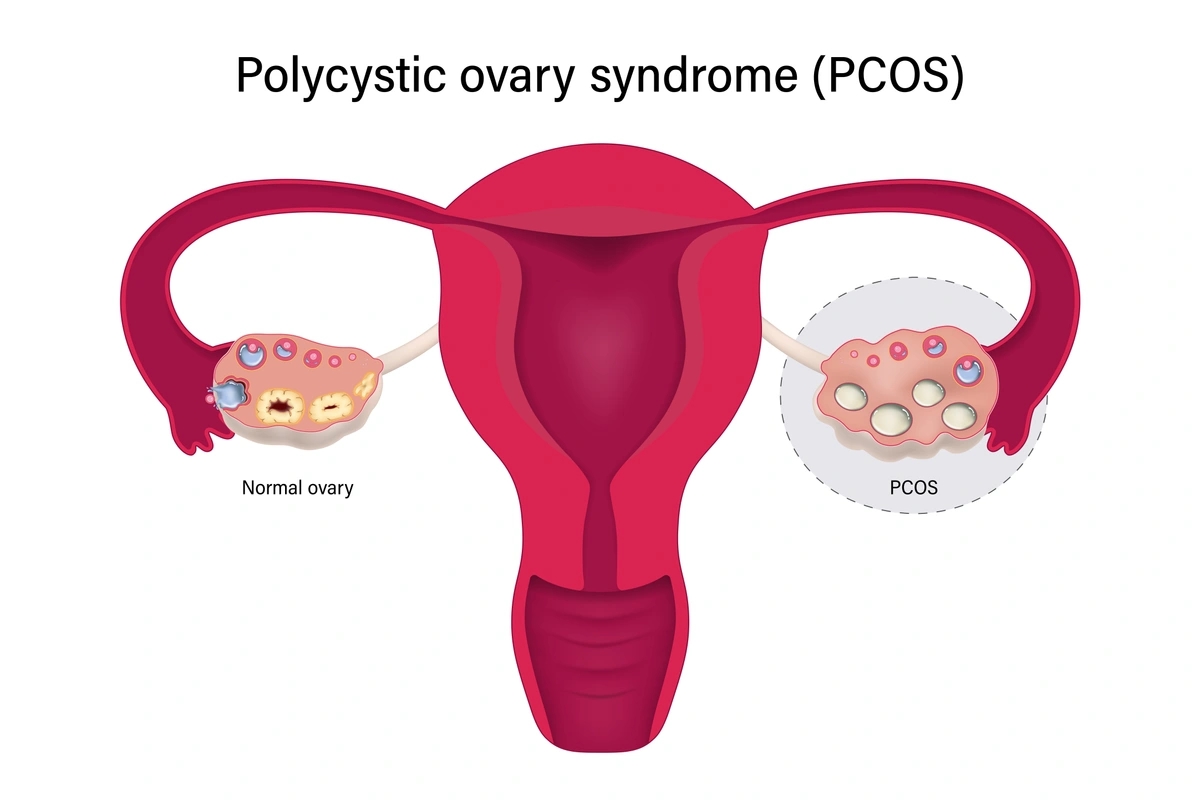
PCOS stands for Polycystic Ovary Syndrome, a condition characterized by a combination of hormonal imbalances, irregular ovulation, and often, polycystic-appearing ovaries.
Unlike a disease that has a single known cause, a syndrome is defined as a group of symptoms that consistently occur together. That’s why PCOS can look very different from person to person. Some patients have obvious symptoms, while others may only discover they have PCOS when they’re trying to conceive.
PCOS can present differently based on age, body type, and reproductive stage. For example:
-
An adolescent with PCOS may struggle with acne and irregular periods.
-
A lean adult may have subtle hormone imbalances.
-
An overweight patient may experience multiple metabolic symptoms.
Illustration of a “normal” ovary and one with PCOS
How is PCOS Diagnosed?
Because PCOS is so variable, several medical organizations have proposed different—but similar—criteria for diagnosis over the past two decades. Most clinicians agree that a PCOS diagnosis requires two of the following three symptoms:
1. Elevated Testosterone Levels (Hyperandrogenism)
PCOS patients often produce higher-than-average levels of androgens (including testosterone). These aren't “male-level” hormone amounts, but they can cause symptoms like:
-
Excess facial or body hair (hirsutism)
-
Acne
-
Hair thinning on the scalp
High testosterone levels also interfere with ovulation, making it harder to conceive.
2. Irregular or Absent Menstrual Periods
At least 80% of individuals with PCOS experience irregular cycles. This is often due to anovulation (not releasing an egg), which significantly impacts fertility.
When left untreated, infrequent periods can also increase the risk of endometrial hyperplasia, a condition where the uterine lining becomes too thick, and, over time, endometrial cancer. That’s why it’s important not to go more than three months without a full menstrual bleed—even when pregnancy isn’t the goal.
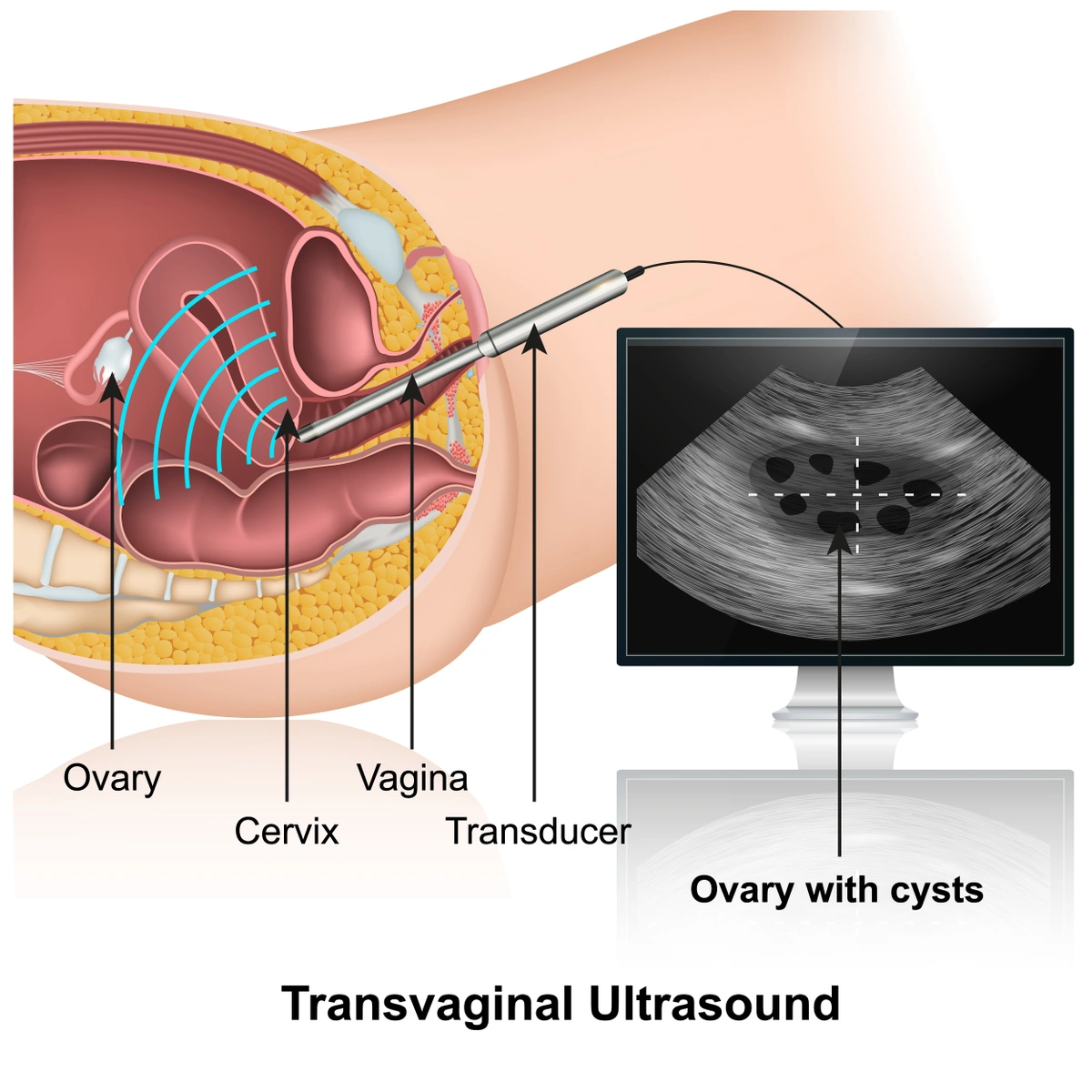
3. Polycystic Ovaries on Ultrasound
Despite the name, “polycystic ovaries” are not actually filled with cysts. What we see on ultrasound are many small immature follicles arranged around the edges of the ovary, giving it a "string of pearls" appearance. These ovaries are often slightly enlarged and may not release eggs properly without medical support.
Illustration of a transvaginal ultrasound of an ovary with cysts
The Link Between PCOS and Insulin Resistance
One of the key drivers behind PCOS is insulin resistance. This means the body doesn’t respond effectively to insulin, leading to elevated blood sugar and insulin levels. Over time, this can increase the risk of:
-
Type 2 diabetes
-
High cholesterol
-
Weight gain
-
Cardiovascular disease
That’s why lifestyle changes—like balanced nutrition, regular exercise, and weight management—are essential parts of PCOS care, even for patients who are not currently trying to conceive.
How PCOS Affects Fertility — And How IFI Can Help
PCOS is one of the most common causes of ovulatory infertility—but the good news is that it’s also one of the most treatable.
At IFI, we offer a range of evidence-based fertility treatments tailored to the unique needs of patients with PCOS, including:
-
Ovulation induction using medications like letrozole or clomiphene
-
In vitro fertilization (IVF) for more complex cases
-
Metformin therapy, in some cases, to support insulin regulation and ovulation
Finding the right medication and dose can take time and fine-tuning, but we’re with you every step of the way to optimize your response and support your goals.
Managing PCOS Beyond Fertility
Even when you’re not actively trying to conceive, managing PCOS is important for your long-term health. Treatment options may include:
-
Hormonal birth control to regulate menstrual cycles and reduce androgen symptoms
-
Lifestyle support for weight management and insulin sensitivity
-
Regular screenings for diabetes and cardiovascular risk factors
When to See a Specialist
If you’re experiencing irregular cycles, unwanted hair growth, persistent acne, or difficulty getting pregnant, it’s a good idea to schedule a visit with a Reproductive Endocrinologist.
At Indiana Fertility Institute, our team specializes in helping patients with PCOS navigate diagnosis, treatment, and fertility planning with compassion and clarity.
You’re not alone—and PCOS doesn’t have to define your future. If you're ready to better understand your symptoms or explore your fertility options, contact IFI to schedule a consultation.